Parent’s Guide: When & How to Seek Mental Health Care for Your Child
20% of Americans live with at least one mental illness. With 50% of these conditions beginning by age 14, and 75% by 24, most people with mental illness experience their first symptoms as a child or teen. Despite these high numbers, less than 14% of children between 5 and 17 receive mental health care, leaving many of them to cope with their conditions without professional treatment until adulthood.
This gap is at least partially due to a nationwide shortage of child & adolescent therapists, with only 4% treating clients under 18. Many children are left to rely on school counselors for help, but there is a lack of these specialists too. The current national average is 1 school counselor for every 1,211 students, which is well above the recommended ratio of 1 to 500. Disparity becomes even greater in rural or low socioeconomic areas, which consistently have even lower rates of available school counselors and local therapists.
It is clear there are many children and teens who live with mental illness, and even more who don’t have access to proper treatment. As difficult as it can be to find help for your child, it is out there, and it’s possible to find it. Reference this guide to learn more about the warning signs of mental health issues in children and teens, and how you can access the care they need to thrive.
Warning Signs of Mental Health Issues in Children & Teens
While there are developmental milestones that we look for as our children grow, they don’t necessarily address mental health concerns. It can be challenging to determine whether certain behaviors are typical. No matter the symptom, your child’s pediatrician can advise if what you’re observing is cause to seek additional support.
These warning signs could be indicative of a mental health issue in children and teens:
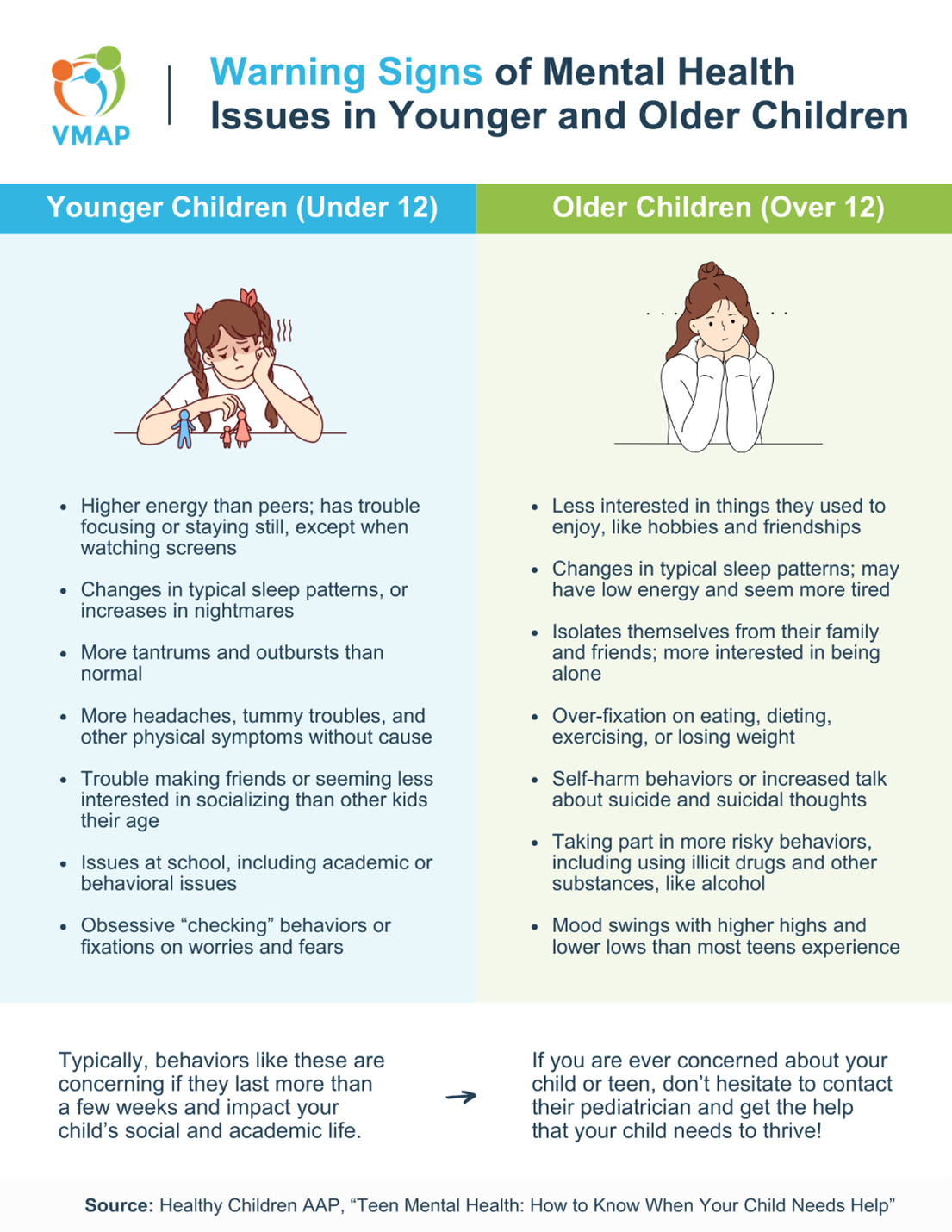
Warning Signs in Children Under 12
- Higher energy than their peers; they may have trouble focusing or staying still, except when they’re occupied with screens
- Changes in their typical sleep patterns, or increases in nightmares
- An increase in tantrums and outbursts
- Complaints of headaches, tummy troubles, or other physical symptoms that don’t seem to have a medical cause
- Difficulty (or lack of interest in) making friends
- Issues at school, including academic or behavioral challenges
- Obsessive behaviors or fixations on their worries and fears
Warning Signs in Children Over 12
- Decreased interest in things they used to enjoy, like hobbies and friendships
- Changes in their typical sleep patterns, or increases in nightmares
- Isolation from family and friends; more interest in being alone
- Fixation on eating, dieting, exercising, or losing weight
- Signs that they are harming themselves; talk of suicidal thoughts, even in passive or joking ways
- Risky behaviors, including drinking alcohol, driving recklessly, or using illicit drugs
- Mood swings and outbursts with higher highs and lower lows than usual
When you speak with your child’s pediatrician about the things you’ve noticed, you want to give them all the information they need. To do this, try to keep track of these three things when you observe a warning sign:
- Intensity: How severe are the symptoms your child is experiencing?
- Duration: How long are the symptoms lasting?
- Distress Level: How much are the symptoms causing your child distress?
Framing your observations with these in mind will help their pediatrician better understand the situation so they can make an informed recommendation.
I’ve Noticed Warning Signs in My Child – Now What?
Speak With Your Child’s Pediatrician
Once you’ve seen one or more consistent and lasting warning signs in your child, speak with their pediatrician to confirm your concerns and learn about the next steps. Some situations may need an environmental adjustment at home or school, while others require professional treatment.
If your child’s pediatrician says that treatment is the way to go, there are a few options they may suggest:
- Assessments: These are often recommended in situations where a pediatrician suspects a specific mental health condition that assessments are available for. However, more general assessments can be performed at therapy intake appointments, and involve an evaluation of your child’s symptoms, as well as their mental, physical, and life history, to get a clearer picture of what’s going on.
- Individual Therapy: There are many different types of therapy, and younger children may benefit from play therapy versus talk therapy. An assessment can help determine which one would work best for your child!
- Family Therapy: This type of therapy is designed to help improve family functioning and communication, often in the wake of an adverse event.
- Group Therapy: This therapy takes place in a group setting with other children who are dealing with similar issues to your child. It relies heavily on peer support.
- Intensive In-Home Services: This is a multi-faceted approach that utilizes crisis intervention, individual therapy, family therapy, and more, and it’s typically used in serious situations where a child is facing an out-of-home placement.
- Inpatient Mental Health Care: This is typically reserved for more severe situations where a child is a danger to themselves or others and needs around-the-clock supervision and care. It’s usually used for short-term crisis intervention.
- Outpatient Mental Health Care: This usually utilizes forms of group therapy, individual therapy, and psychiatry to help address your child’s problems in an intensive way, but lets them continue living at home versus a treatment center. It’s only used when your child isn’t responding to regular therapy and needs something more, but they are stable enough to stay safe during treatment.
- Psychiatry: Finding a child and adolescent psychiatrist (CAP) is tough, but your pediatrician can call the VMAP Line to connect with a CAP about your child’s case. Not every child is the right candidate for psychiatric medication, but a CAP will be able to assess the situation and determine a course of action.
If you’re feeling uncomfortable bringing up the topic of mental health treatment with your child, you can ask their pediatrician if they can help facilitate this conversation during an office visit. Even if you are confident in navigating this initial conversation alone, it may be helpful to ask their pediatrician for developmentally appropriate ways to introduce treatment to your child without making it sound negative or like a punishment.
Find Mental Health Treatment for Your Child
When it comes to finding a therapist, we’ve rounded up some resources below to help you get started. (If you’ve been referred to seek intensive in-home treatment, inpatient/outpatient care, or psychiatry, your child’s pediatrician should be able to help!)
Search Directories
While you could try and use the front page of Google to find a child therapist, there are some websites that have been specifically created to help you do this in a more direct way! Many of these let you search for therapists by insurance plan, mental health issues, ages they treat, and more, which can help narrow down your choices. If you think your child would be a good candidate for telehealth therapy (i.e., they’re developmentally able to focus on therapy during a Zoom call, communicate with their therapist in this format, and make progress), you can expand your search to therapists across Virginia. Here are some websites where you can get started!
Referral Resources
If you’d rather start offline, there are several places you can seek referrals for local therapists:
- Your Child’s Pediatrician
- Your Child’s School Social Worker/Counselor
- Friends + Family
- Local Community Groups
- Your Health Insurance (call to find in-network providers!)
Your child’s pediatrician can also utilize the VMAP Line to receive care navigation and referrals for your child’s case, if needed.
However you decide to search for a child therapist, it’s wise to try out a few. Most therapists have an initial intake session, where you and your child can talk about your reasons for starting therapy. This session is a fantastic opportunity to ask some of the screening questions below, which can help you determine if this therapist is the right fit for your child. Make sure you leave space and time for your child to ask questions as well!
Suggested Screening Questions:
- What’s your background and training working with children?
- What age range do you usually work with?
- What type of therapeutic methods do you use with children/teens?
- How often do you meet with parents? Do you want me and my child to both be in sessions together?
- Will you be in contact with my child’s teacher/school counselor?
- How long do children usually stay in therapy with you?
- Are you familiar with [your child’s issue]?
- Are you providing telehealth, in-person, or a combination of session types?
Once you’ve settled on a therapist, encourage your child to be open with you if they feel like they’re not connecting with their therapist or making progress after a few sessions. It may be challenging to find a therapist who’s a great fit for your child – but don’t give up! If you must go back to the drawing board, return to the resources listed earlier to try again.
As always, VMAP is committed to expanding access and education for Virginia healthcare providers who treat children and adolescents. We hope that our efforts mean that more children and teens get the right support, treatment, and referrals for their mental health needs.