Dating Violence Among Teens: How Pediatricians Can Support Patients
Prevalence of Dating Violence & Abuse in Teen Relationships
It’s estimated that 19% of teenagers experience sexual or physical dating violence, 50% deal with stalking and harassment, and 65% have been psychologically abused in a relationship (Office of Juvenile Justice and Delinquency Prevention). Even though these numbers seem astronomical, they may be even higher—it’s estimated that only about 1/3 of teens report their experiences of dating violence.

There are also notable gender differences in teen dating violence. Even though both teen boys and girls alike are impacted by dating violence, and much of this violence is mutual, it’s reported that boys are more likely to resort to sexual violence, and girls are more likely to act out psychological violence. Ethnicity and sexual orientation are also a factor—those who identify as Native North American, Hawaiian/Pacific Islander, and LGBTQ+ experience the highest rates of teen dating violence.
No matter who experiences dating violence, its victims can be impacted by long-lasting harm for years to come. When compared to teens who don’t experience dating violence, those that do are at higher risk of:
- Doing poorly in school, both socially and academically
- Developing codependent / overly dependent tendencies with others
- Entering violent & abusive relationships as an adult
- Engaging in risky sexual behaviors
- Exhibiting antisocial behaviors (such as lying, stealing, bullying, fighting, and violence)
- Developing mental health conditions (including substance use disorders, anxiety, depression, and eating disorders)
- Experiencing self-harm, suicidal ideation, and suicide attempts
Sources: CDC, Office of Juvenile Justice and Delinquency Prevention, Youth.gov
The Role of the Pediatrician
Pediatricians may be wondering where they fit into this picture. After all, you are part of your patient’s journeys throughout their development, and that includes adolescence! When it comes to dating violence and teen relationships, pediatricians play a role in four major ways:
- Educating teens and their caregivers about the warning signs of an unhealthy relationship
- Creating a safe, private, and confidential space for teens during their visit with you
- Screening teens (especially high-risk ones) for dating violence and abuse
- Supporting teens and connecting them to resources when they disclose that they are experiencing dating violence and abuse
Below, we walk through each of these one by one, providing research and resources along the way. Our hope is that by the end, you will feel more prepared to support your pediatric patients around the tough subject of dating violence.
1. Educate Teens & Caregivers About Unhealthy vs. Healthy Relationships
While some relationships start off with blatantly abusive behaviors, it’s more common for unhealthy tendencies to begin subtly and worsen into abuse and violence as time goes on. Awareness is key—if teens and their parents aren’t aware of the many forms that abuse and violence can take, it can be easy to miss. Taking the time to educate your teen patients and their parents about healthy vs. unhealthy relationships is a great way to do your part in preventing dating violence.
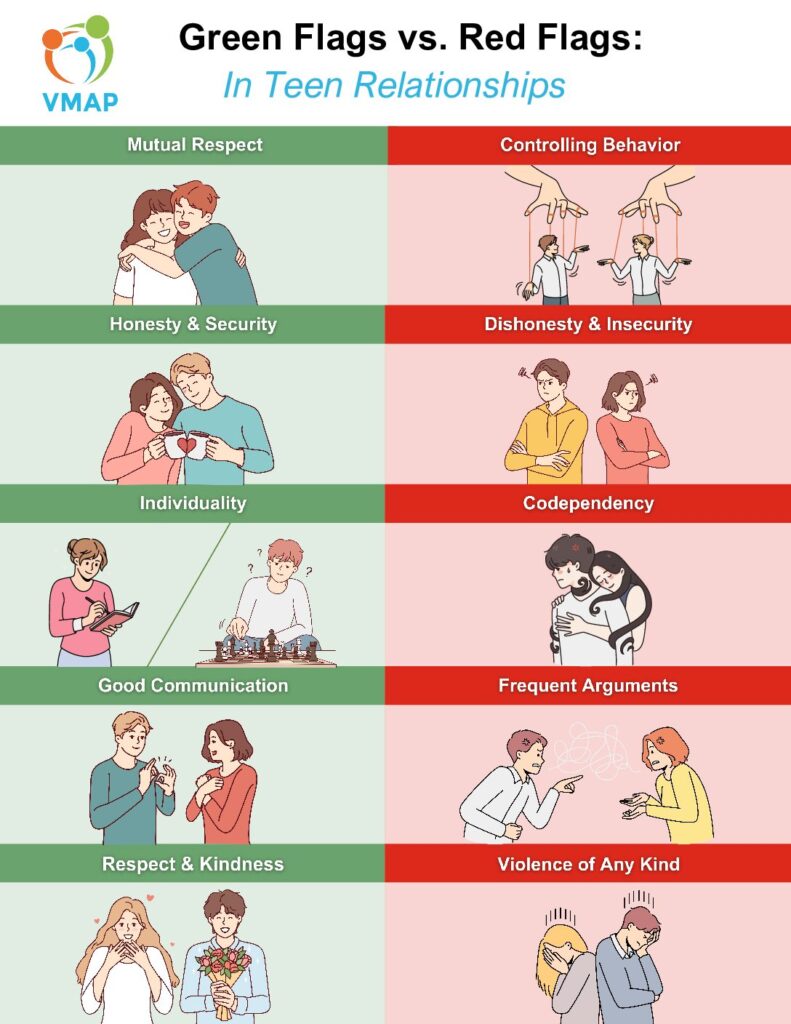
Below is a printable handout you can give to your patients and their families to summarize what we see as “green” or “red” flags in a teen relationship. This is a fantastic resource to keep handy at your practice!
2. Provide a Safe, Confidential Space for Teens to Share Their Experiences
Many teens need a safe space. As much as we would love for every home to be one, that’s not always the case. Even if teens openly communicate with their parents and feel comfortable doing so, there may still be some things that they are hesitant to share. As a result, 1/3 of teens say they would refuse to seek healthcare for sensitive health concerns if they felt like their parents could find out. When they are sure that confidentiality is going to be respected during their visit, they are more likely to seek healthcare services, return for follow-ups, and disclose information about risky behaviors.
As pediatricians, it can be challenging to navigate the complexities of confidentiality with minors, especially if your teen patient has disclosed to you that they are experiencing dating violence. Your instinct may be to involve the parents, but teens typically have the right to keep this between the two of you. Once puberty begins, most pediatricians build optional alone time with their young patient into the visit. During their alone time, the pre-teen or teen can talk to you about anything they’d like, and unless they disclose that they or someone they know is in danger, transmitted infections, mental health issues, substance abuse, pregnancy, and sexual assault can be withheld from parents, if the teen does not give you explicit permission to share these things with them.
If you’ve ever felt confused about the limits of confidentiality, you’re not alone—77% of physicians, including those in family medicine and pediatrics, report that they need additional training on confidentiality laws. To help, we have a tip sheet for practitioners on confidentiality laws from the American Academy of Pediatrics (AAP), and a list of current legal requirements for provider confidentiality in Virginia.
Once you have a thorough understanding of confidentiality, it’s critical that you share this information with your patients. Taking the time to explain confidentiality and its limitations has been shown to encourage open communication with teens, even around sensitive health concerns. It’s equally important to ensure your teen patients get one-on-one time with you, so they can discuss sensitive issues away from their parents. Some may want their parents to stay in the room, especially younger teens, and that’s okay—but providing that option and establishing a routine early can help build trust with your patient for future visits.
3. Use Dating Violence Screening Tools and Questions to Assess Teens
Despite high rates of teen dating violence, many report not being screened for this during their pediatric visits. If you want to incorporate screenings for dating violence in your practice, there are a few screening tools you can use to help identify unhealthy or abusive relationships in teens. The most common one is the HEADSSS Assessment (see a tip sheet here and an implementation guide), and you can also ask your patient these general screening questions from Stanford Medicine.
While there isn’t a long list of options available for teen-specific screening tools on this subject, studies have shown that simply asking a few direct questions about safety, experiences of physical violence, and feelings of fear in relationships can correctly identify dating violence in many teens.
While it would be ideal to screen every teen who visits you, this isn’t a realistic endeavor for all pediatric practices. If your practice has limited resources, teens in the following groups should be the priority for dating violence screening:
- Teens with past exposure to domestic violence, including through their parents
- Teens who use or abuse drugs and/or alcohol
- Teens who are experience symptoms of anxiety, depression, or other mental illness
- Teens with irregular or inconsistent history of medical care and visitation
- Teens who participate in risky sexual behaviors
- Teens with concerning responses to the dating violence screening tools or questions
If you are hoping to incorporate universal screening for dating violence into your practice, experts recommend that you implement this in conjunction with an educational piece. This would involve helping your patient understand why the screening is being done, what resources are available to them, and confidentiality limits.
Additionally, providers at your practice would need to be prepared to connect patients with resources after a dating violence disclosure. This step is crucial, as studies have found that implementing universal screening on its own doesn’t improve resource usage or overall outcomes in teens.
4. Follow Up Dating Violence Disclosure with Resources and Support
If a teen shares with you that they are experiencing any kind of abuse or violence in their relationship, your next steps should be done with warmth, understanding, and the teen’s safety at the forefront. Providing a rote list of resources without this warm approach has been demonstrated to be insufficient and ineffective.
A hand-off should start with thanking the teen for sharing their situation with you. After this, tell them that you can connect them with someone to talk through available resources. Some pediatric practices may have an on-site social worker or a victim advocate for this purpose. However, if you have limited or non-existent access to this kind of support, you can suggest national resources and hotlines such as:
- National Domestic Violence Hotline (Call: 1-800-799-7233 / Text: 88788)
- Love Is Respect Hotline (Call: 1-866-331-9474 / Text: 22522)
- Any resource listed here by the National Sexual Violence Resource Center
Depending on your comfort level, you can also work with the teen to develop a safety plan, like this one from Love is Respect. If the teen is open to it and gives explicit permission, you can also involve and educate their parents on how to help their child through this. AAP has developed this list of tips for parents who have a teen experiencing dating violence.
We hope this article has helped you feel more prepared to address teen dating violence with your patients. As a reminder, if you need additional support for a pediatric patient who is facing a mental health crisis or concern (including because of dating violence), you can call the VMAP Line and get connected to a mental health professional to assist you in providing informed care for your patient!