The State of Child Mental Health Care in Virginia
22% of children and teens across America live with one or more mental health conditions, and this number is on the rise. Rates of childhood anxiety and depression rose by 29% and 27% between 2016 and 2020, and there was a 34.6% increase in pediatric mental illnesses as a whole between 2012 and 2018. This situation was exacerbated by the COVID-19 pandemic, which saw a 25% rise in anxiety and depression across the globe. During this time, emergency rooms saw record highs of pediatric patients coming in for mental health reasons (+24% for children ages 5-11, +31% for those ages 12-17), which coincided with staggering numbers of suspected teen suicide attempts.
The Child & Adolescent Mental Health Crisis
All of this led the American Academy of Pediatrics (AAP), the American Academy of Child and Adolescent Psychiatry (AACAP), and the Children’s Hospital Association to declare a national emergency in children’s mental health in 2021. They called on policymakers, mental health experts, and primary care providers (PCPs) to take action and address this crisis. Unfortunately, nationwide gaps in mental health care access for children made this much easier said than done.
In Virginia, this gap is acutely felt. Our state ranks 48th lowest in the country when it comes to youth mental healthcare access, and 97 localities are mental health professional shortage areas. Only 4 counties have enough child and adolescent psychiatrists to serve their populations, and overall, there are only 14 of these specialists available for every 100,000 children in Virginia. This severe shortage of mental health experts often leaves youth and their parents to either face eternal waitlists or be turned away entirely—which is where PCPs come into the picture.
Many patients with symptoms of mental illness will see their PCPs first to address the issue, often before they have been able to see a mental health expert or get a diagnosis. For children and teens, this PCP is usually their pediatrician. Unfortunately, pediatricians and other PCPs who see pediatric patients are not usually prepared to help in these situations. In fact, over 65% of pediatricians say they lack the necessary training, knowledge, and skills in pediatric mental health, often leaving them at a loss on how to best support these patients.
With rates of childhood mental illness on the rise, limited access to mental health specialists, and overwhelmed PCPs unable to find the time or funds to gain new skills in pediatric mental health, Virginia needed more support—and that’s why the Virginia Mental Health Access Program (VMAP) was created!
Two Ways VMAP Closes the Gap in Child Mental Health Care
-
The VMAP Line
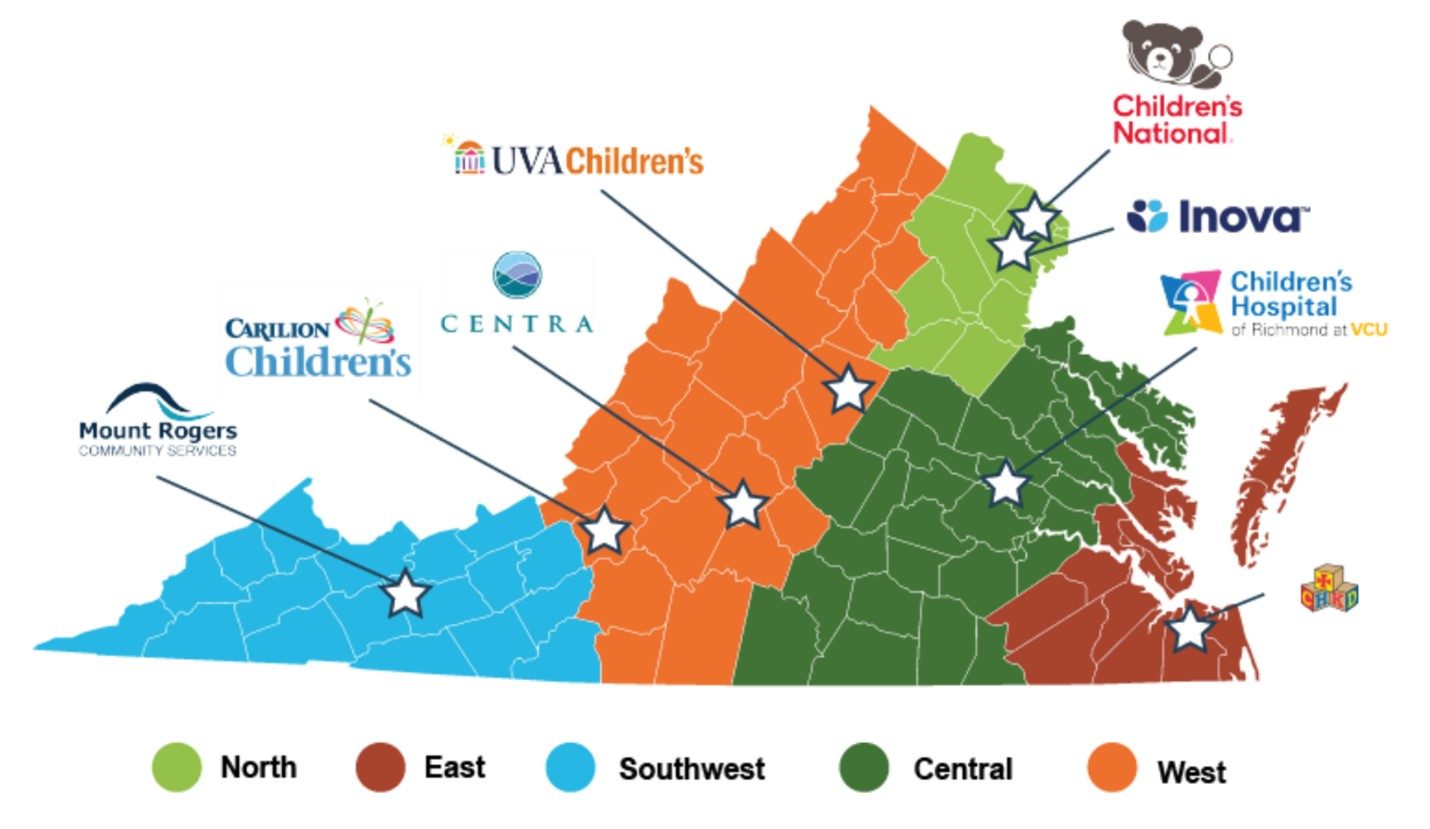
VMAP provides a solution to the current crisis in two major ways. The first is through the VMAP Line, which is staffed by mental health specialists across Virginia. We are able to achieve this statewide coverage thanks to our partnerships with regional hospital systems, which serve as hubs where the VMAP Line operates.
The VMAP Line offers free same-day consultation to any Virginia PCP who treats children or adolescents (0-21) and needs help regarding their patient’s mental health. These PCPs can connect with experts like:
- Child & Adolescent Psychiatrists
- Developmental Pediatricians
- Licensed Mental Health Professionals
Additionally, Virginia PCPs can request care navigation, either as part of their consultation or separately. Care navigation helps their pediatric patients connect with local mental health resources and referrals. This service is invaluable, especially for PCPs who work in areas where such resources are scarce.
2. Provider Education
Each year, VMAP puts on a variety of expert-led pediatric mental health training with optional CME and/or MOC credit. These opportunities are designed to be low or no cost and convenient for PCPs with busy schedules. Our core offerings include:
- REACH: Mini-fellowship followed by case-based distance learning.
- ECHO: Monthly virtual cohorts with tracks for specialized interests.
- Pearls & Pitfalls: Bi-monthly webinars on critical and PCP-requested topics.
Each training is meant to leave PCPs feeling more confident when diagnosing, treating, and managing pediatric mental health. Acquiring these critical skills means more Virginia PCPs are better equipped to address situations that arise in their daily practice. If they ever feel out of their depth, the VMAP Line is prepared to assist with consultations and care navigation!
VMAP’s Impact Across Virginia
In the last 4 years, VMAP has made a real impact in Virginia. Here are just a few of our achievements, which are possible thanks to our partners, leadership, staff, and PCPs across the state!
Trained over 1,100 PCPs with our provider education offerings

Received more than 6,600 calls from providers to the VMAP Line
Virginia PCPs, click here to call the VMAP Line!
Served 5,600 Virginia pediatric patients through VMAP Line consultations
The Future of VMAP
As VMAP continues to gain support, our services are growing. Right now, there are two expansions in the works; one for early childhood mental health, and another for perinatal mental health!
- Early Childhood Expansion
In 2023, VMAP received state funding to extend our services into early childhood mental health, focusing on children under the age of 6. Studies have shown that 16% of children under the age of 6 face significant mental health challenges that are difficult to resolve without intervention. Despite this, most of the limited resources in Virginia are directed toward older children and teens, leaving these younger children vulnerable.
The first part of VMAP’s Early Childhood Expansion added new developmental/behavioral pediatricians, and care navigators. We also began offering new trainings on early childhood mental health, including Early Childhood ECHO cohorts, learning collaboratives, and a Triple P training pilot.
- VMAP for Moms+
In 2024, VMAP acquired funding to develop services for maternal health providers who see pregnant and postpartum patients, which includes OB/GYNs, family physicians, midwives, and more. 20% of patients report having mental health issues during pregnancy or postpartum, but 75% never receive treatment. Perinatal mental health issues are the leading cause of maternal mortality in America, and left untreated, they can lead to preterm delivery, difficulty bonding with the child, and much more.
In response, VMAP is planning to launch several perinatal efforts this summer. Perinatal psychiatrists, LMHPs, and care navigators who all specialize in this branch of mental health will join the VMAP Line. We will also add perinatal mental health training to our rotating education offerings, with the hope to train maternal health providers on screening, diagnosing, and managing perinatal mental health conditions
With the continued support of our partners and PCPs, we are excited to see what else VMAP will achieve this year. If you want to have a hand in supporting our efforts, you can start by spreading the word about VMAP—you can use these outreach materials to do it!